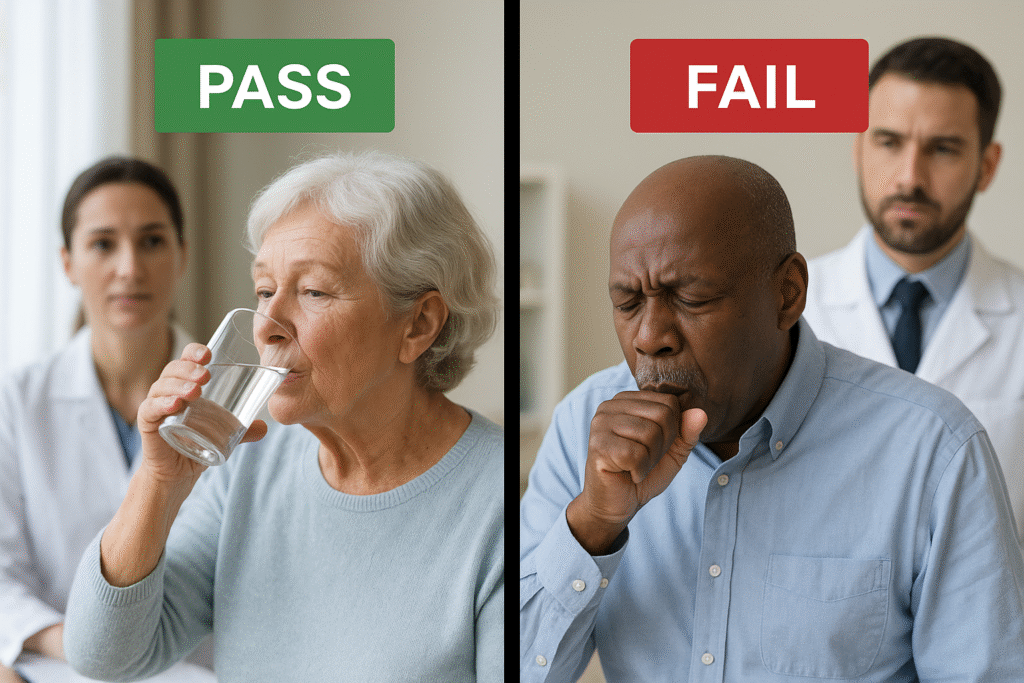
When a patient shows signs of swallowing difficulty, clinicians often begin with a simple but high-stakes question: Can this person safely eat or drink? “Pass/fail” dysphagia screenings exist to help answer that question quickly. They help determine whether oral intake is likely safe or if further testing is needed to assess safety of swallowing, allowing teams to act before aspiration or malnutrition risks escalate.
As highlighted in Clinical and Instrumental Swallowing Assessments for Dysphagia (NCBI Bookshelf, Haas, 2024), these screenings are designed for rapid triage. They are the first step in a layered process of identifying dysphagia and guiding next-level evaluation with instrumental tools such as FEES or VFSS.
What Pass/Fail Dysphagia Really Means
A pass/fail screen looks for visible or audible signs of aspiration, things like coughing, throat clearing, or a wet, gurgly voice. A “pass” suggests no immediate signs of aspiration and allows cautious oral intake. A “fail” signals potential danger, prompting clinicians to keep the patient NPO and refer for further assessment.
This binary outcome might sound basic, but it serves a critical role in protecting patients and prioritizing limited resources. It’s particularly valuable in acute care and post-stroke settings, where quick decisions can prevent aspiration pneumonia and expedite rehabilitation.
Common Screening Tools and Their Clinical Impact
One of the most widely validated tools is the 3-ounce Water Swallow Test (WST), in which the patient drinks water continuously while the clinician observes for coughing or vocal changes. Research by Kuuskoski et al., 2024 in The Laryngoscope found the WST to have sensitivity rates exceeding 96 percent for aspiration prediction confirming its continued value as a fast and reliable bedside measure.
The Yale Swallow Protocol, validated by Suiter and colleagues, standardizes the WST for hospital use, reducing variability and improving referral consistency to speech-language pathologists for confirmatory testing. Meanwhile, the Geriatric Bedside Swallowing Screen (GEBS), currently under validation in JMIR Research Protocols (Javorszky et al., 2023), is adapting the model for older adults, comparing bedside results directly with FEES outcomes to improve accuracy in geriatric populations.
Pass/fail screenings are only the first step. When a patient fails or when subtle symptoms persist despite a pass the next move is instrumental assessment. FEES and VFSS allow clinicians to visualize the anatomy and physiology of swallowing, revealing the mechanisms behind aspiration or residue that a bedside exam cannot detect.
In many cases, FEES provides greater accessibility and precision. It offers a real-time, color view of the laryngeal and pharyngeal structures during the swallow, capturing even silent aspiration events. As Haas (2024) notes, combining a screening, and following up with an instrumental study remains the gold standard for ensuring safety and tailoring treatment.
Understanding the Limitations
No screening tool, no matter how validated, replaces direct visualization. A “pass” result can miss silent aspiration; a “fail” might restrict patients who could safely eat. Overreliance on bedside screens can lead to both under- and over-management of dysphagia, emphasizing the need for confirmatory imaging whenever possible.
The Diagnostic Value of FEES
At DiagnosTech FEES, our mobile endoscopic swallowing evaluations bridge that gap. We bring hospital-grade instrumentation directly to your facility, allowing for immediate, objective assessment following bedside screening. FEES not only confirms whether aspiration is occurring, but clarifies why helping clinicians develop personalized treatment strategies that restore safety and quality of life.
To learn how FEES can enhance your dysphagia screening protocol or complement your bedside assessments, contact us.
